The Deeptech Revolution Reshaping Women’s Health
By Alexandra | April 9, 2025
FemTech is revolutionising the way we approach women’s health. Efforts to increase gender representation in the workforce have brought forward an increasing awareness of unique health and everyday challenges faced by women. This has also led to the destigmatisation of topics related to menstruation, menopause, sex-specific health conditions and representations, as well as challenges faced by both sexes, such as fertility.
These shifting paradigms are creating fertile ground for a progressive, fast-growing FemTech industry, capturing the attention of scientists, entrepreneurs, and investors alike. This has led to exponential growth in published FemTech scientific articles, FemTech start-ups and venture capital (VC) funding rounds. FemTech start-ups have also shown the ability to secure significant late funding stages, including Flo’s Series C, Maven Clinic’s Series D and Progyny’s IPO, reaching valuations above $1 billion (McKinsey and Company, 2022).
The DeepTech revolution is now shaping this landscape, driven by groundbreaking scientific advances in biomarker and drug discovery, regenerative medicine and digital health. This transformation is not just a response to unmet medical needs, it is a step towards closing the long-standing health gap, and it poses the question of whether the next FemTech unicorn will be born from deeply scientific innovations.

The Health Data Gap
Sex specific differences in disease prevalence, diagnosis, severity, outcomes, treatment efficacy and adverse side effects are being increasingly recognised. However, a significant data gap exists in understanding the origins and implications of these differences. This gap stems from historical biases in clinical research, where female participants were often excluded due to concerns over hormonal variability, leading to a lack of comprehensive data on differential effects of treatments in women. As a result, many pharmaceuticals that have been approved based on male-dominated trials exhibit altered pharmacokinetics and pharmacodynamics in women, increasing the risk of adverse drug reactions, suboptimal dosing regimens and differences in clinical trial outcomes (Spoletini et al., 2012). Furthermore, conditions that predominantly affect women, such as autoimmune diseases or women-specific diseases such as endometriosis and polycystic ovary syndrome (PCOS), have been historically underfunded and understudied, compounding the knowledge deficit.
Advances in computational modelling, digital twins, and sensor technology are expected to enable a more precise and individualised approach to women’s health research. Digital twins, machine learning-driven virtual representations of individual patients, allow for the simulation of physiological responses under different treatment conditions, providing a sex-specific framework for drug discovery and personalised medicine. Additionally, clinical trials are increasingly incorporating sex-stratified analyses to refine treatment approaches and mitigate historical biases in drug development.
The emergence of wearable biosensors and real-time tracking devices is further transforming data collection by enabling continuous, non-invasive monitoring of physiological parameters such as hormonal and temperature fluctuations, metabolic rates, sleep cycles, and cardiovascular health. These technological advancements not only address the longstanding data gap in women’s health but also hold the potential to revolutionise precision medicine by integrating sex-specific biomarkers into therapeutic development and clinical decision-making. Such advancements are particularly attractive for pharmaceutical companies and contract research organisations seeking to maximise the outcomes and opportunities of their drug development programmes, opening new avenues for enhanced drug development programs and significant revenue opportunities for innovative start-ups.
Hidden diagnostic opportunities in menstrual blood
For a long time considered one of nature’s most stigmatised fluids, menstrual blood was largely ignored as a biological sample. However, it has emerged as a valuable source of health information and biomolecules, offering critical insights into reproductive health and common systemic, high-burden conditions. For example, endometriosis, characterised by chronic pain, inflammation, scarring and heavy bleeding, is historically difficult to diagnose due to the invasiveness of the procedure. Recent studies indicate that biomarkers found in menstrual blood can enable non-invasive diagnosis of endometriosis, potentially reducing the need for surgical diagnostic methods and bridging the gap between symptoms and diagnosis (Riski Amanda et al., 2024; Starodubtseva et al., 2024). Moreover, menstrual blood can be used to monitor other chronic conditions, such as diabetes, thyroid disorders, cervical cancer, and menopause. Research has shown a high correlation between biomarkers in circulating blood and menstrual blood, for example, HbA1c levels for diabetes prognosis, offering a non-invasive alternative to traditional blood tests (Naseri et al., 2022).

Additionally, the endometrial tissue, which regenerates monthly without scarring, contains menstrual stem cells (MenSCs). These cells, which can be collected non-invasively from menstrual blood, possess a high proliferative capacity and pluripotency comparable to bone marrow-derived stem cells. They can differentiate into various cell types, including neurons, cartilage, fat, bone, heart, liver, and skin cells. Importantly, these stem cells can also regenerate endometrial cells, potentially repairing damaged uterine tissue and improving fertility.
Collectively, these insights underscore a massive opportunity for innovation in women’s health. By harnessing the unique properties of menstrual blood, researchers and clinicians can develop groundbreaking diagnostic tools and therapeutic strategies that enhance our understanding of systemic health and transform the management of reproductive disorders. This paradigm shift opens up new frontiers for personalised medicine and represents an exciting, untapped resource that could revolutionise healthcare for millions worldwide.
Fertility technologies
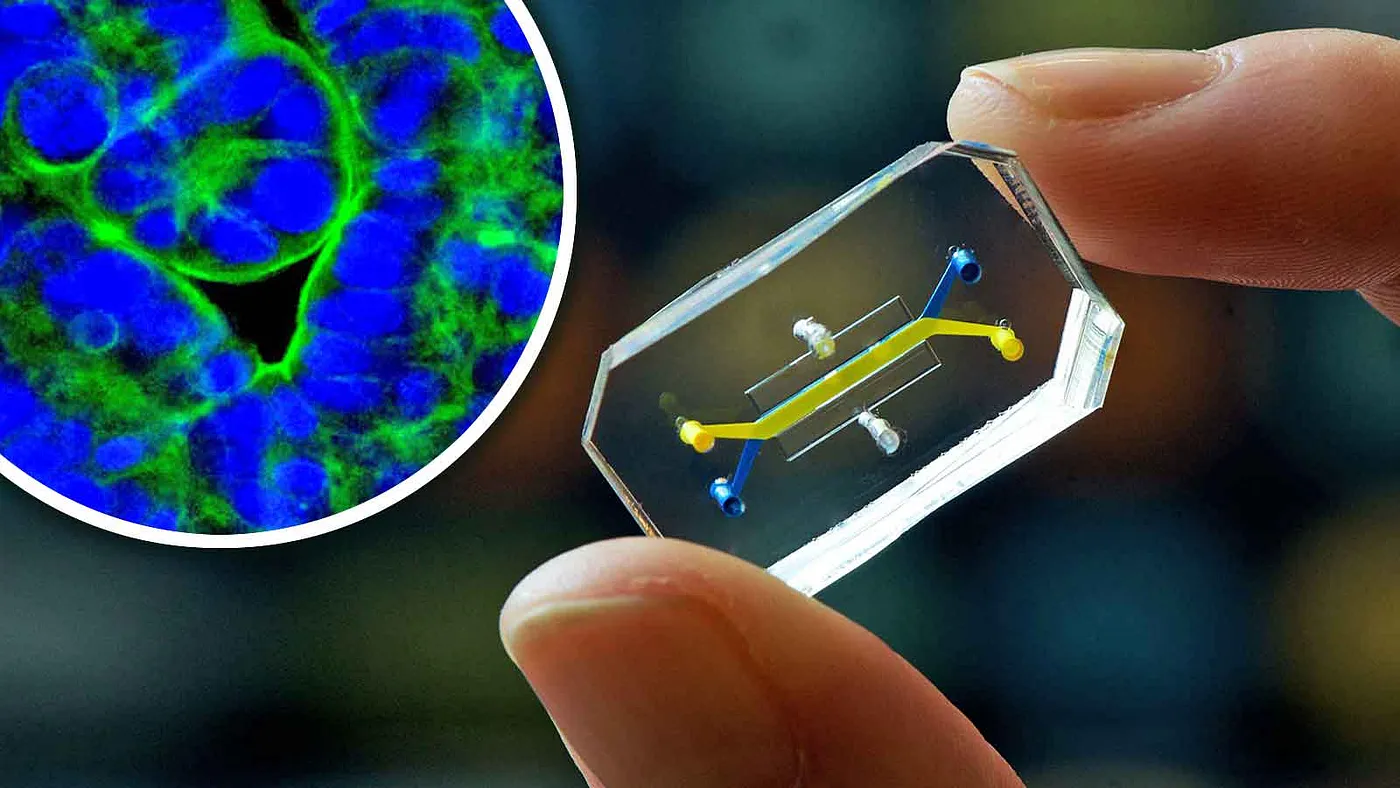
With falling birth rates, the fertility industry is receiving increasing attention as researchers and clinicians work to address both male and female factors in infertility. For men, novel technologies such as ML-assisted sperm analysis and sorting, microfluidic sorting techniques, and at-home sperm testing kits are enhancing our ability to assess and optimise sperm quality. Meanwhile, female fertility is often complicated by conditions that have long been challenging to study, including premature ovarian insufficiency, polycystic ovary syndrome (PCOS), endometriosis, and various hormonal imbalances. Gaining a deeper understanding of these diseases is essential for developing more effective in vivo interventions, which represents a significant opportunity for both research and clinical innovation.
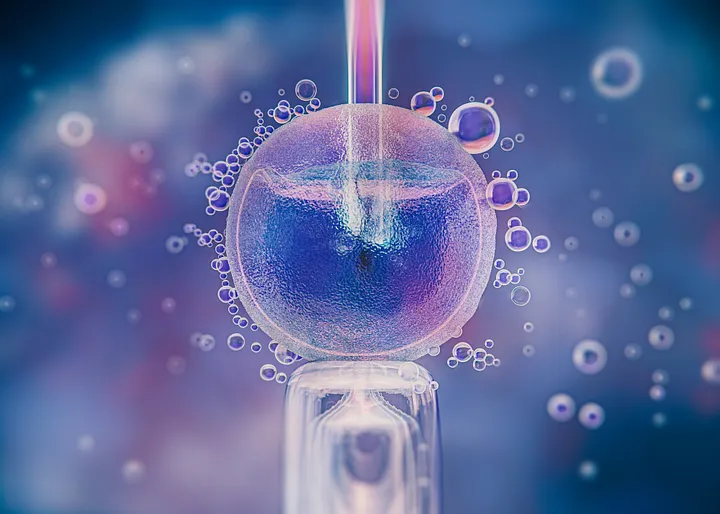
In vitro fertilisation (IVF) remains a cornerstone of reproductive medicine, yet it is not without its challenges. Hormonal stimulation protocols required for IVF can be physically and emotionally taxing for women, while success rates continue to be modest and treatment costs can be prohibitive. These challenges have received significant academic and industrial attention in the past decades, and we believe that numerous scientific breakthroughs will reach commercialisation in the near future. These include advances in embryo selection, non-invasive methods for assessing oocyte and sperm quality, and advances in lab-grown gametes, their stimulation and ovarian tissue preservation.
The growth of these technologies is supported by the strategic investments and novel funding models of many start-ups and scale-ups. However, the access to advanced fertility treatments and continuous technological progress will remain influenced by geography, as countries show varying degrees of public support and regulation.
Reproductive ageing
Reproductive ageing refers to the age-related functional decline in both male and female reproductive systems, compromising fertility and leading to a range of health complications. In women, this process is characterised by a decrease in the quantity and quality of oocytes stored in ovarian follicles, eventually culminating in menopause, the natural cessation of menstrual cycles. While often viewed as merely the end of fertility, reproductive ageing has far-reaching implications for overall health, affecting metabolism, cardiovascular function, cognitive abilities, and bone health.
With increasing life expectancy, there is an exciting opportunity to develop therapeutics that delay the ageing process and prolong ovarian life. Strategies aimed at extending the ovarian healthspan focus on preserving ovarian function, improving the quality of oocytes, and modulating the hormonal changes that occur during ageing. Advanced diagnostic tools that detect early biomarkers of reproductive ageing are also emerging, enabling the timely application of these innovative therapies.
This shift towards proactive and preventive care not only holds the promise of enhancing fertility and delaying menopause but also offers the potential to reduce the broader systemic health risks, such as metabolic and cardiovascular issues, associated with ageing. By extending ovarian function and overall reproductive health, these novel therapeutic strategies are expected to transform how we manage reproductive ageing, paving the way for improved quality of life and long-term wellbeing. Moreover, recent developments have demonstrated that modulating key molecular pathways can preserve oocyte quality and delay ovarian ageing, underscoring the potential for targeted deeptech interventions in this space (Zielinska et al., 2015).
Challenges faced by the FemTech industry
Despite the rapid momentum in FemTech, the sector faces significant barriers, causing a lag behind other developing industries and skepticism among some (Forbes Technology Council, 2023). Regulatory uncertainty is one of the most pressing challenges, as in vivo interventions ranging from fertility treatments to hormone-based therapies and AI-powered diagnostics are uniquely challenged by the organisation of clinical and pre-clinical trials and the high burden of proof of safety and efficacy. Additionally, the global landscape is highly fragmented, with inconsistent regulatory frameworks and funding infrastructures across different regions. These disparities often limit access to innovative digital health solutions and cutting-edge fertility treatments, ultimately creating an uneven playing field for emerging FemTech startups.
Compounding these challenges are investment gaps and long-standing societal biases that have historically stifled progress in women’s health. Many promising solutions remain underfunded due to a combination of risk-averse investment cultures and lingering stigmas surrounding topics like menstruation, menopause, and fertility. However, these hurdles also present unique opportunities for advocacy and reform. By establishing clearer, harmonised regulatory pathways, fostering greater investment diversity, and addressing cultural taboos through public awareness, stakeholders can accelerate the pace of innovation in FemTech. In doing so, the industry can not only overcome its current obstacles but also expand access to more inclusive, effective healthcare solutions for women worldwide.
The Future of FemTech:
The FemTech revolution represents far more than a market opportunity, it marks a long-overdue transformation in healthcare that is redefining how we understand, treat, and invest in women’s health. Despite historical neglect, rapid scientific breakthroughs in machine learning, biometrics, reproductive medicine, and digital health are steadily closing the data gap and challenging outdated paradigms.
While regulatory hurdles, funding disparities, and geographic inconsistencies continue to pose challenges, the momentum behind FemTech is undeniable. As emerging technologies push the boundaries of what is possible, the future of women’s health is set for unprecedented advancements, promising more inclusive and effective care for millions worldwide.
Kristina Kordova is a PhD in Biological Sciences at Cambridge University and the lead of Creator Fund’s Life Science Team. Nayanika Bhalla is a PhD in Biotechnology at KTH in Stockholm and a Venture Fellow at Creator Fund.
References
- McKinsey and Company. 2022. The dawn of the FemTech revolution. https://www.mckinsey.com/industries/healthcare/our-insights/the-dawn-of-the-femtech-revolution
- Spoletini, I., Vitale, C., Malorni, W., & Rosano, G. M. C. (2012). Sex differences in drug effects: Interaction with sex hormones in adult life. Handbook of Experimental Pharmacology, 214, 91–105. https://doi.org/10.1007/978-3-642-30726-3_5
- Riski Amanda, C., Asmarinah, Hestiantoro, A., Tulandi, T., & Febriyeni. (2024). Gene expression of aromatase, SF-1, and HSD17B2 in menstrual blood as noninvasive diagnostic biomarkers for endometriosis. European Journal of Obstetrics & Gynecology and Reproductive Biology, 301, 95–101. https://doi.org/10.1016/J.EJOGRB.2024.07.061
- Starodubtseva, N., Chagovets, V., Tokareva, A., Dumanovskaya, M., Kukaev, E., Novoselova, A., Frankevich, V., Pavlovich, S. v., & Sukhikh, G. (2024). Diagnostic Value of Menstrual Blood Lipidomics in Endometriosis: A Pilot Study. Biomolecules, 14(8), 899. https://doi.org/10.3390/BIOM14080899/S1
- Naseri, S., Leung Brewster, R. C., & Blumenthal, P. D. (2022). Novel use of menstrual blood for monitoring glycaemic control in patients with diabetes: a proof-of-concept study. BMJ Sexual & Reproductive Health, 48(2), 123–127. https://doi.org/10.1136/BMJSRH-2021-201211
- Zielinska, A. P., Holubcova, Z., Blayney, M., Elder, K., & Schuh, M. (2015). Sister kinetochore splitting and precocious disintegration of bivalents could explain the maternal age effect. ELife, 4(DECEMBER2015). https://doi.org/10.7554/ELIFE.11389
- Alexandr Khomich for Forbes Technology Council. 2023. The Growth Of FemTech: Separating Hype From Facts. https://www.forbes.com/councils/forbestechcouncil/2023/12/21/the-growth-of-femtech-separating-hype-from-facts/